What happens to our bodies after we die? Far from shutting down instantly, science reveals a fascinating “twilight of death” where certain cells and processes persist, some for minutes, others for days. Brain and nerve cells perish within minutes without oxygen, while skin and corneas can remain viable for a full day, and white blood cells endure up to three days. Even more astonishing, gene transcription—where DNA segments are copied into RNA—continues for hours or days after clinical death. This postmortem activity raises profound questions, especially for organ transplantation, as researchers now link this “twilight” to an increased cancer risk in transplant recipients. Could the body’s final biological gasps hold hidden dangers for modern medicine? Let’s explore this eerie frontier and its implications for transplants.
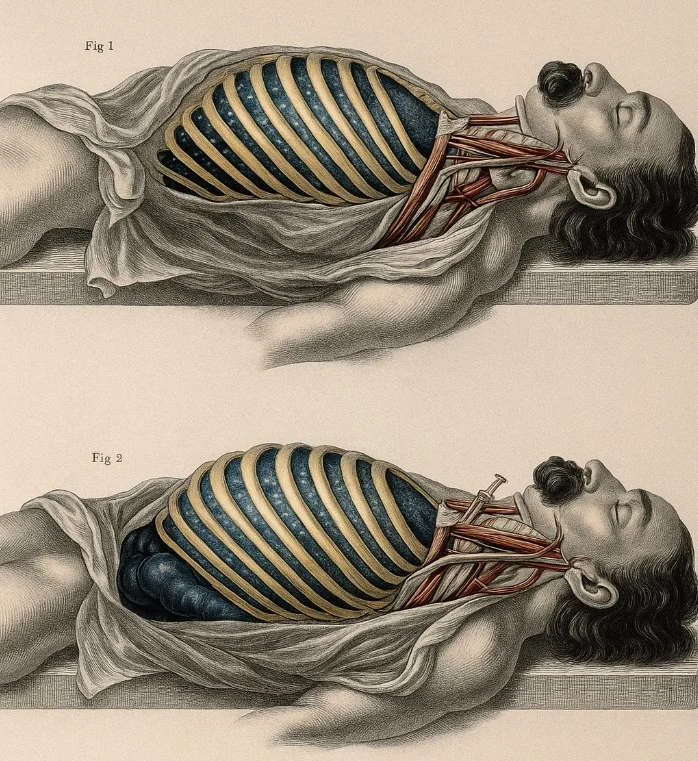
When breathing stops, the body’s cells don’t all die at once. The brain and nerve cells, voracious oxygen consumers, begin to falter within minutes, unable to sustain their complex functions. The heart, liver, kidneys, and pancreas follow, surviving for about an hour before succumbing to oxygen deprivation. Remarkably, other tissues are far more resilient. Skin, tendons, heart valves, and corneas remain viable for up to 24 hours, while white blood cells can persist for three days. This staggered timeline of cellular survival is critical for organ and tissue transplantation, allowing doctors to harvest viable components long after clinical death, defined as the cessation of heartbeat and breathing.
Yet, the most intriguing discovery lies in what scientists call the “twilight of death.” Far from a silent shutdown, the body enters a period of continued biological activity. Research published in journals like Nature and Science has shown that gene transcription, a process where cells copy DNA segments into RNA to produce proteins, persists in certain cells for hours or even days postmortem. This activity isn’t random; it involves genes linked to stress responses, inflammation, and even developmental processes, as if the body is mounting a final, futile defense against death. In studies on deceased mice and zebrafish, researchers observed heightened activity in genes associated with wound healing and immune responses, suggesting cells are reacting to the stress of oxygen loss in a state of “blind panic.”
This postmortem gene activity has profound implications for organ transplantation, a field that saves over 40,000 lives annually in the U.S. alone. Organs like hearts, livers, and kidneys, harvested within an hour of death, and tissues like corneas, preserved for up to a day, are critical to transplant medicine. However, transplant recipients face a well-documented risk: a significantly higher incidence of cancer, with studies estimating a 2-4 times greater likelihood compared to the general population. The reasons are complex, involving immunosuppressive drugs that weaken cancer-fighting defenses and the stress of organ integration. But emerging research points to a chilling new factor: the twilight of death itself.
Scientists hypothesize that the frenetic gene transcription in dying cells could alter their DNA in ways that promote oncogenesis—the formation of cancer. During the twilight period, surviving cells may activate stress-related genes, leading to mutations or epigenetic changes (alterations in gene expression without changing the DNA sequence). When these cells are transplanted into a living body, they may carry a latent “cancer risk” that manifests under the recipient’s immunosuppressive regimen. For example, a 2018 study in Transplantation found that donor-derived cancers, where the transplanted organ itself develops malignancy, are rare but linked to cellular stress responses in the donor tissue. The longer tissues remain viable postmortem, like corneas or white blood cells, the more time they have to undergo these risky changes.
The implications are both scientific and ethical. Organ transplantation relies on the delicate balance of timing—harvesting organs quickly to ensure viability while minimizing cellular damage. The twilight of death complicates this calculus. For instance, heart valves and corneas, viable for 24 hours, may accumulate more genetic alterations than kidneys, which are typically transplanted within an hour. White blood cells, surviving up to three days, could pose an even higher risk if used in grafts or transfusions. Researchers are now exploring whether these postmortem changes can be mitigated, perhaps by cooling tissues faster to slow gene activity or screening donor organs for stress-induced mutations.
This discovery also challenges our understanding of life and death. The persistence of gene transcription blurs the line between the two, suggesting that death is not a singular event but a process. Philosophically, it raises questions about when a body is truly “gone” and whether transplanted tissues carry a vestige of the donor’s biological identity. For transplant medicine, it underscores the need for advanced diagnostics. Current protocols focus on matching blood types and tissue compatibility, but future standards may include genetic profiling to assess postmortem gene activity. Such innovations could reduce cancer risks and improve outcomes for recipients, who already face a 50% chance of organ rejection within 10 years.
The broader medical context amplifies the urgency of this research. With over 100,000 people on the U.S. transplant waiting list and a global shortage of donor organs, maximizing the safety and efficacy of transplants is critical. The rise of xenotransplantation (using animal organs) and bioengineered tissues adds further complexity, as these methods may also involve cells with unpredictable postmortem behavior. Public awareness is growing, with social media platforms buzzing about the “twilight of death” and its implications. Transplant recipients and donor families are particularly vocal, seeking clarity on risks and advocating for safer protocols.
For the public, this science is both fascinating and unsettling. The idea that cells continue “working” after death evokes awe and unease, while the cancer link raises concerns about a life-saving procedure. Yet, it also highlights the resilience of the human body, with cells fighting to survive even in the face of mortality. As researchers delve deeper, they aim to harness this knowledge to refine transplantation, potentially saving more lives while minimizing risks. The twilight of death, once a scientific curiosity, is now a frontier with real-world stakes.
The “twilight of death” reveals a haunting truth: our bodies continue to function long after we’re gone, with gene transcription persisting in a final act of biological defiance. This discovery, while awe-inspiring, casts a shadow over organ transplantation, linking postmortem cellular activity to increased cancer risks in recipients. As brain cells die within minutes and corneas endure for a day, the staggered survival of tissues shapes the transplant landscape, but the twilight period’s genetic chaos demands new safeguards. With science probing the boundaries of life and death, this phenomenon challenges medicine to evolve. Can we protect transplant patients from these hidden risks? Will the twilight of death redefine how we save lives? The answers lie ahead, and the world is watching. Let’s talk science!